The Intricate Link Between Obesity and Cancer
In recent decades, the global prevalence of obesity has reached alarming levels, emerging as a significant public health concern. With this surge in obesity rates, researchers have turned their attention to the intricate relationship between obesity and cancer risk. Scientific and medical studies have consistently demonstrated a compelling connection between excess body weight and an increased susceptibility to various forms of cancer. Understanding the mechanisms underlying this relationship is crucial for devising effective preventive strategies and interventions.
Obesity is a Growing Epidemic
The World Health Organization (WHO) defines obesity by a body mass index (BMI) greater than or equal to 30. According to the Global Burden of Disease Study, obesity has more than tripled since 1975, affecting over 650 million adults worldwide in 2016. This rapid increase has raised concerns not only due to its association with chronic conditions like diabetes and cardiovascular diseases but also because of its intricate link to cancer.
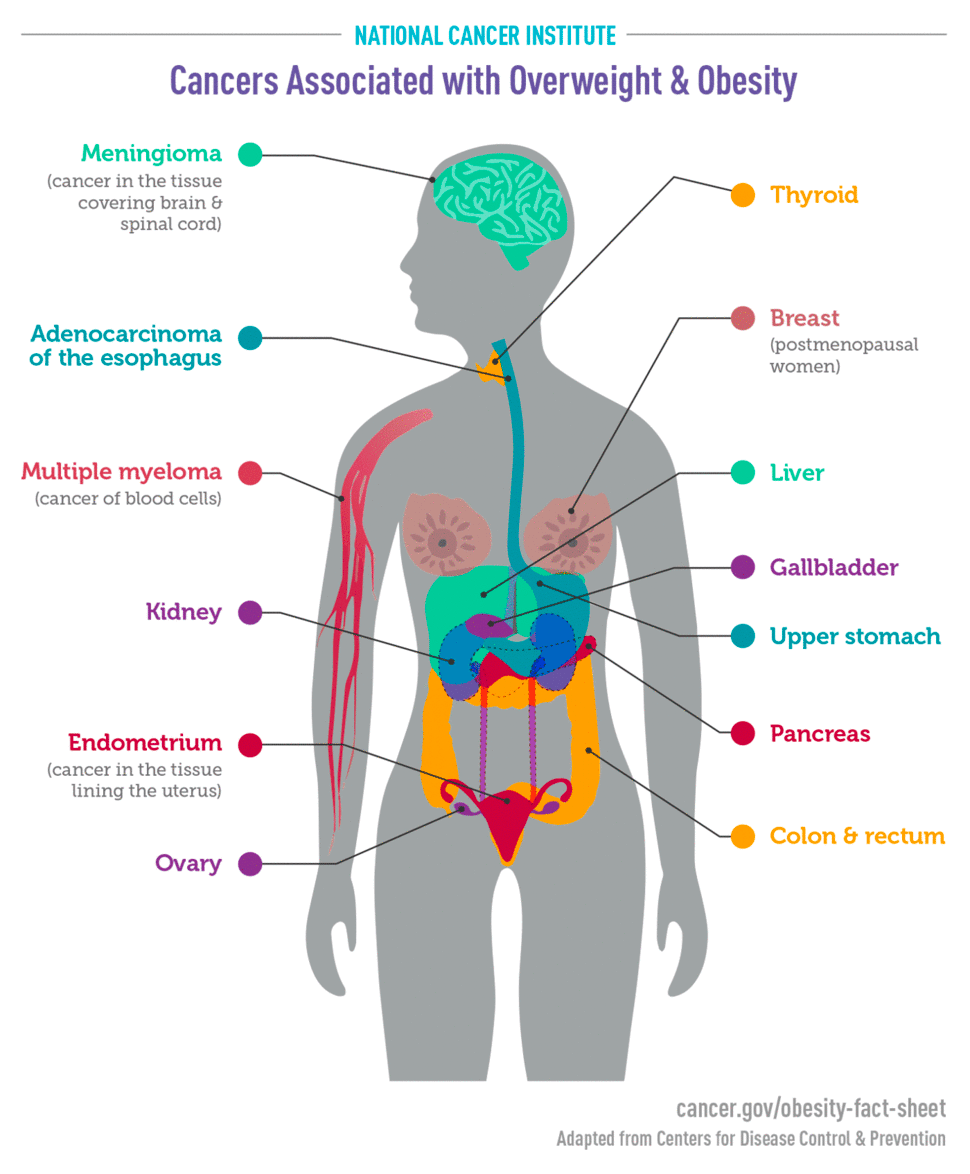
Obesity has been linked to 13 types of cancer
Medical and epidemiological studies have consistently reinforced the connection between obesity and cancer risk. According to research from the American Cancer Society, excess body weight is thought to be responsible for about 11% of cancers in women and about 5% of cancers in men in the United States, as well as about 7% of all cancer-related deaths.
The CDC reports that overweight and obesity have been linked to 13 cancers, including breast cancer, cancer of the kidneys, and thyroid cancer.
 Breast Cancer:
Breast Cancer:
Among women, postmenopausal breast cancer has garnered substantial attention in the context of obesity. Adipose tissue is known to produce estrogen, and the excess estrogen produced in obese individuals can stimulate the growth of hormone receptor-positive breast cancer cells. Moreover, the chronic inflammation associated with obesity creates an environment conducive to cancer cell growth and metastasis.
Colorectal Cancer:
Obesity has been closely linked to an increased risk of colorectal cancer. Studies have shown that obesity is associated with insulin resistance, a condition in which the body's cells become less responsive to insulin, resulting in elevated insulin levels. This insulin resistance can fuel the growth of colorectal cancer cells, as insulin promotes cell proliferation and inhibits apoptosis (programmed cell death).
Endometrial Cancer:
Obesity is considered a major risk factor for endometrial cancer, which affects the lining of the uterus. Similar to breast cancer, excess estrogen produced by adipose tissue plays a pivotal role in the development of endometrial cancer. Furthermore, obesity-induced insulin resistance and chronic inflammation contribute to the progression of this cancer type.
Kidney Cancer:
Renal cell carcinoma, the most common form of kidney cancer, has also demonstrated a correlation with obesity. Adipose tissue produces cytokines, which are signaling proteins that can promote cell proliferation and angiogenesis, the formation of new blood vessels that supply tumors with nutrients. These cytokines are believed to foster the growth and spread of kidney cancer cells.
How obesity increases cancer risk
Numerous scientific studies have provided compelling evidence that obesity significantly increases the risk of developing several types of cancer. The exact mechanisms driving this relationship, however, are multifaceted and complex. Some potential ways obesity increases the risk of cancer include:
- Increased fat tissue— Adipose tissue, commonly referred to as fat tissue, emerges as a key player in this connection. It produces excessive quantities of estrogen, a hormone recognized for its involvement in cancer development. Elevated estrogen levels have been directly linked to escalated risks of various cancers, such as breast, endometrial, ovarian, and certain other malignancies.
- Increased insulin levels— Within the context of obesity, a cascade of metabolic changes unfolds. Those living with obesity frequently exhibit heightened blood concentrations of insulin and insulin-like growth factor-1 (IGF-1). Hyperinsulinemia, a condition arising from insulin resistance, often precedes the onset of type 2 diabetes—a well-established cancer risk factor. Studies have found that elevated insulin and IGF-1 levels have the potential to foster the progression of cancers like colon, kidney, prostate, and endometrial cancers.
- Higher levels of inflammation— Compounding the intricate web of obesity-related mechanisms are chronic inflammatory conditions that frequently accompany obesity. Conditions like gallstones or non-alcoholic fatty liver disease (NAFLD) induce oxidative stress, a phenomenon that triggers DNA damage. Consequently, the risk of gallbladder cancer (and similar biliary tract cancers) is heightened.
- Increase in molecules that causes cells to grow and divide— Adipose or fat tissue secretes pro-inflammatory molecules known as adipokines. These molecules can stimulate or inhibit cell growth, which, in turn, may make cancer more likely. Take leptin, for instance—an adipokine whose presence in the bloodstream surges alongside increasing body fat. Elevated levels of leptin can cause aberrant cell proliferation (meaning, there’s more opportunity for cancerous cells to develop in the body). Conversely, another adipokine, adiponectin, appears to be less abundant in those with obesity compared to individuals within a healthy weight range. This is important because adiponectin has antiproliferative properties, meaning it might act as a safeguard against tumor growth.
- Other molecular effects—Furthermore, the complex fat cells can also increase the production of molecular pathways, like the mammalian target of rapamycin (mTOR) and AMP-activated protein kinase. These pathways hold the potential to directly or indirectly influence cell growth and metabolism. For example, mTOR may be more active in some types of cancer cells than it is in normal cells. And blocking mTOR may cause the cancer cells to die.
- Weakened immune system— Intriguingly, obesity's potential impact on cancer risk isn't solely confined to molecular and physiological interactions. The multifaceted nature of this relationship might extend to the immune system's vigilance against tumors and even alterations in the structural characteristics of the tissue surrounding burgeoning tumors. See, e.g., this 2015 study that explored this phenomenon in breast cancer.
- Worsened screenings and medical care for those with obesity— Beyond its intricate biological effects, obesity can also lead to challenges in terms of cancer screening and management. A prime example lies in the realm of cervical cancer. Women with overweight or obesity face an elevated risk of cervical cancer when compared to their counterparts with a healthier body weight. This increased risk is partly attributed to the potentially less effective cervical cancer screening techniques employed in these individuals. This means that those with obesity might not have their cancer detected as often.
In essence, the interwoven network of mechanisms linking obesity to cancer risk paints a complex picture. Adipose tissue's multifaceted role, encompassing hormone secretion, inflammation, and intricate molecular interactions, underscores the need for a comprehensive understanding of this connection. Additionally, the implications of obesity on cancer screening further highlight the urgency of reducing weight stigma in medicine and improving comprehensive weight health care.
Treating obesity can reduce cancer risk
Weight loss holds the potential to significantly decrease the probability of developing specific types of cancers.
The American Cancer Society emphasizes the importance of maintaining a healthy weight in reducing cancer risk. Their recommendations align with those of various other health organizations, which advocate for the importance of weight management, a balanced diet, and physical activity in cancer prevention.
By actively pursuing weight loss and maintaining a lower body weight, people can proactively mitigate the risk factors associated with cancer. A study published in The Lancet in 2016 analyzed data from over 10 million adults and found a strong positive association between BMI and the risk of developing various cancers. The researchers observed that for each 5 kg/m² increase in BMI, there was an associated increase in the risk of several cancers, including pancreatic, kidney, ovarian, and colon cancers.
Furthermore, in a 2022 study published in JAMA, researchers followed over 30,000 adults with obesity across a few years. The study's findings highlighted a significant correlation between weight loss from bariatric surgery and reduced cancer risk. Those who underwent weight loss surgery had a 32% decrease in the likelihood of developing cancer and a 48% lower risk of dying from cancer when compared to a similar group of people who did not undergo surgery.
Over the study's duration, participants who opted for weight loss surgery lost an average of 55 pounds more than their counterparts who did not have surgery. The researchers found that the more weight loss corresponded to a higher decrease in cancer risk. More research is still needed to fully explore the implications of weight loss on cancer prevention.
Implications for public health:
The growing body of evidence linking obesity and cancer risk underscores the need for comprehensive public health strategies. Awareness campaigns, educational initiatives, and policy changes are all critical components of combating the obesity epidemic and its associated cancer risk. Such efforts might focus on encouraging healthier lifestyles that incorporate balanced diets and regular physical activity, educating about new weight health treatments, and building community infrastructure that supports wellness. Schools, workplaces, and communities play vital roles in promoting environments conducive to healthier choices.
Moreover, healthcare professionals must be equipped with the knowledge and resources to address obesity and its potential consequences—while being free of weight bias. Clinicians should routinely assess patients' weight status, provide guidance on weight management, and offer personalized recommendations for reducing cancer risk. Integrated care models that combine the expertise of healthcare providers, dietitians, and fitness professionals can prove highly effective in addressing the multifaceted nature of obesity.
Conclusion:
The complex relationship between obesity and cancer risk is a significant concern for global public health. Scientific and medical research has consistently shown that obesity fosters a pro-inflammatory environment, contributes to insulin resistance, and elevates hormone levels, all of which can fuel the initiation and progression of various cancer types. As the prevalence of obesity continues to rise, the importance of understanding and addressing this link cannot be overstated.
Preventive measures and interventions should be a priority for individuals, healthcare systems, and policymakers alike. Encouraging and facilitating healthier lifestyles, raising awareness about the risks associated with obesity, and promoting early intervention are essential steps in mitigating the impact of obesity on cancer incidence. By tackling the obesity epidemic, we not only improve overall well-being but also take a substantial stride toward reducing the burden of cancer on society.